The sympathetic system is involved in the fight, flight, fright, and sex response.
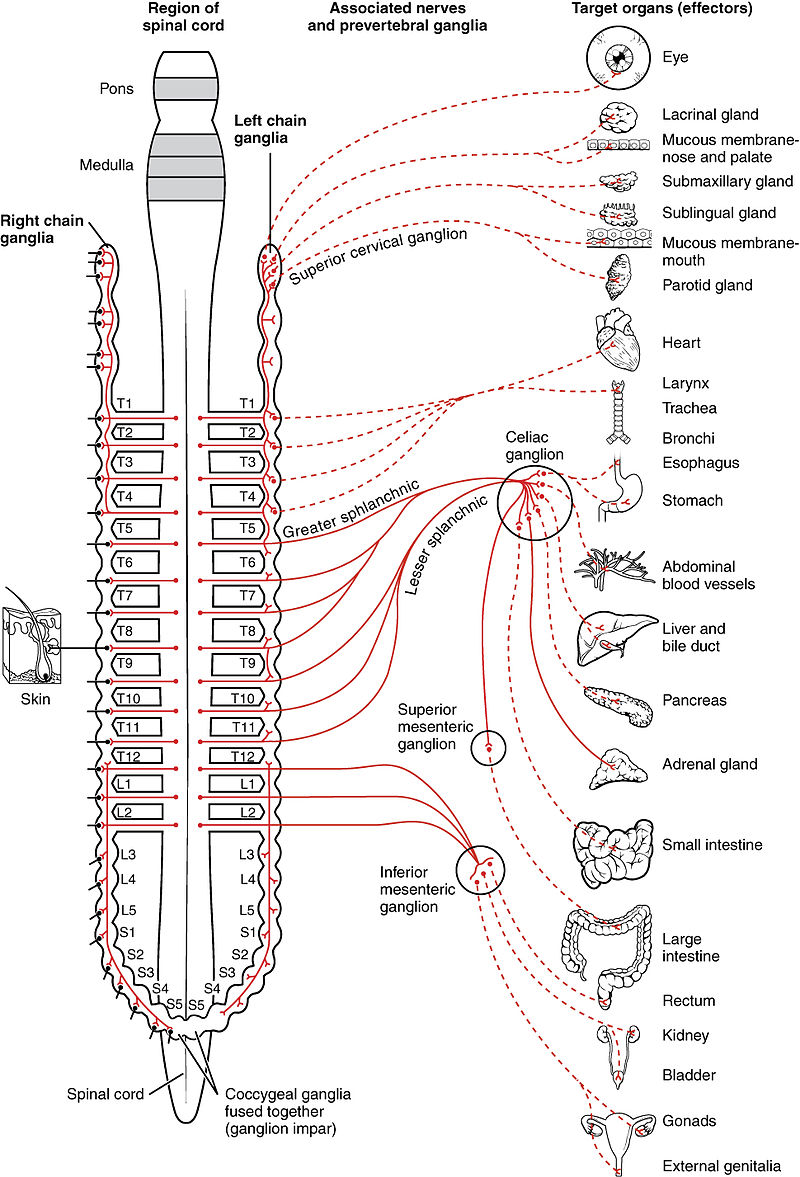
Cell bodies of the sympathetic preganglionic neurons are located in the lateral horn of the spinal cord gray matter between T1-L2.
Their axons traverse the ventral horn to exit in ventral roots where they form synapses onto postganglionic neurons.
The preganglionic axons form synapses with many postganglionic cells, thus giving this system a widespread action. The neurotransmitter of the preganglionic axons is acethylcholine.
The postganglionic neurons are located lateral to the vertebral column in the thoracic and lumbar regions.
The neurotransmitter of the postganglionic neurons is norepinephrine,
The sympathetic nervous system exerts its effect through alpha (α) and beta (β) receptors in the target organs.
> alpha (α) and beta (β) receptors
alpha (α)
-
α 1 Receptors act as smooth muscle constrictors, meaning that they tighten sphincters and also contract the smooth muscles of arterioles in the circulatory system (vasoconstriction), increasing systemic vascular resistance and raising blood pressure. The goal of this vasoconstriction is to decrease blood flow to nonvital areas and redirect it to skeletal muscle to support activity. Those parts of the body that are less vital to be perfused during activity will have more of these receptors, causing more vasoconstriction in these areas. In addition, the pupillary dilator muscle in the eye has α 1 receptors, which cause dilation of the pupil to allow more light in during the fight-or-flight response. Phenylephrine is a pure α 1 agonist that clamps down blood vessels, often used to raise blood pressure in hypotensive patients in the operating room and also used to stop runny noses constricting vessels in the nose to stop vascular congestion.
-
α 2 Receptors act as negative feedback to keep the sympathetic response regulated. Clonidine is an α 2 agonist and therefore through negative feedback has the net effect of decreasing sympathetic outflow , which is beneficial in the treatment of hypertension. Clonidien is more commonly used to manage the sympathetic nervous system activation surges that often accompany opiate withdrawal in patients attempting to quit their addiction.
beta (β) receptors .
β 1 Receptors are found mostly on the heart and act as cardiac stimulants . They mainly increase the rate (chronotropy) and contractility (inotropy) of the heart, allowing for increased cardiac output and delivery of blood to tissues to support their increased activity during one of those four Fs. Beta blockers work by preventing activation of this receptor, which ensures that the heart doesn’t work too hard (require more oxygen) in patients with heart disease. In patients with heart failure, prolonged sympathetic activation actually causes long-term remodeling and changes in the heart that are maladaptive—beta blockade also helps prevent this neurohumoral remodeling.
Beta-adrenoceptor agonists (β-agonists) bind to β-receptors on cardiac and smooth muscle tissues.
They also have important actions in other tissues, especially bronchial smooth muscle (relaxation), the liver (stimulate glycogenolysis) and kidneys (stimulate renin release).
Beta-adrenoceptors normally bind to norepinephrine released by sympathetic adrenergic nerves, and to circulating epinephrine.
Therefore, β-agonists mimic the actions of sympathetic adrenergic stimulation acting through β-adrenoceptors. Overall, the effect of β-agonists is cardiac stimulation (increased heart rate, contractility, conduction velocity, relaxation) and systemic vasodilation.
Arterial pressure may increase, but not necessarily because the fall in systemic vascular resistance offsets the increase in cardiac output. Therefore, the effect on arterial pressure depends on the relative influence on cardiac versus vascular β-adrenoceptors.
Long-term exposure to β-agonists can cause β-receptor down-regulation, which limits their therapeutic efficacy to short-term application. Beta-agonists, because they are catecholamines, have a low bioavailability and therefore must be given by intravenous infusion.
Beta-agonists bind to beta-adrenoceptors located in cardiac nodal tissue, the conducting system, and contracting myocytes.The heart has both β1 and β2 adrenoceptors, although the predominant receptor type in number and function is β1. These receptors primarily bind norepinephrine that is released from sympathetic adrenergic nerves. Additionally, they bind norepinephrine and epinephrine that circulate in the blood.
Beta-adrenoceptors are coupled to Gs-proteins, which activate adenylyl cyclase to form cAMP from ATP. Increased cAMP activates a cAMP-dependent protein kinase (PK-A) that phosphorylates L-type calcium channels, which causes increased calcium entry into the cells. Increased calcium entry during action potentials leads to enhanced release of calcium by the sarcoplasmic reticulum in the heart; these actions increase inotropy (contractility). Gs-protein activation also increases heart rate by opening ion channels responsible for pacemaker currents in the sinoatrial node. PK-A phosphorylates sites on the sarcoplasmic reticulum, which enhances the release of calcium through the ryanodine receptors (ryanodine-sensitive, calcium-release channels) associated with the sarcoplasmic reticulum. This provides more calcium for binding the troponin-C, which enhances inotropy. Finally, PK-A can phosphorylate myosin light chains, which may also contribute to the positive inotropic effect of beta-adrenoceptor stimulation. In summary, the cardiac effects of a β-agonist are increased heart rate, contractility, conduction velocity, and relaxation rate.
- ❍
β 2 Receptors act as smooth muscle relaxers , which seems counterintuitive when contrasted with α 1 receptors. However, it is the location of these receptors that is important—to increase blood flow to skeletal muscle, more β 2 receptors instead of α 1 receptors are found on arterioles feeding skeletal muscles. In addition, β 2 receptors are found on the bronchioles of the lung, and activation of these receptors relaxes smooth muscle in this area, allowing for better airflow during breathing—which is why the β 2 agonist albuterol is so effective in treating asthma. You have 1 heart (β 1 works on the heart), and you have 2 lungs (β 2 works on the lungs).
Signal Transduction Pathways
All of the aforementioned receptors (and all receptors) need to trigger some sort of signal transduction pathway to relay the message and start the cascade that eventually causes the intended effect of the receptor.
The most common pathway for this is through G-protein-coupled receptors (GPCRs) , which are also known as seven-transmembrane domain receptors because they cross the cell membrane seven times. There are many subtypes of GPCRs, each of which has a different downstream pathway—it is important to understand the G q , G s , and G i pathways (only three!). Now that you understand what each receptor of the sympathetic nervous system does, it is time to move on to how it does it, through these GPCRs.
GPCRs have α, β, and γ subunits and are active when a signal molecule (e.g., a neurotransmitter or drug) attaches to the receptor and causes the α subunit to exchange its bound inactive guanosine diphosphate (GDP) for an active guanosine triphosphate (GTP)—this activates the α subunit to in turn activate the βγ complex, which will then go on to activate whatever downstream pathway is involved, depending on whether or not it goes through the G q , G s , or G i pathway. The α subunit has a GTPase, which will eventually hydrolyze one of the phosphates off of GTP to change it back to inactive GDP, to ensure that the signal doesn’t continue going on forever. (Note: these α and β are subunits of the GPCR—different from the α and β sympathetic nervous system receptors discussed previously!)
-
G q : The G q pathway has the end result of increasing calcium levels in the targeted cells; in the case of the α 1 receptors on the arterioles of blood vessels, the calcium surge causes contraction of those muscles and therefore causes vasoconstriction. The exact mechanism of how calcium release allows muscular contraction is covered in Chapter 12 in detail. Refer to the graphic that depicts the G q pathway: the active βγ complex activates phospholipase C, cleaving the PIP 2 molecule into IP 3 and diacylglycerol (DAG). The IP 3 binds to a special channel on the sarcoplasmic reticulum (an organelle in smooth muscle cells that holds calcium to be ready for contraction) and releases that calcium. DAG, on the other hand, can be made into prostaglandins, which regulate pain and inflammatory responses, and also activates protein kinase C (PKC), which can phosphorylate other molecules and exert other effects ( Fig. 7-7A ).
-
G s : The G s pathway has the end result of activating protein kinase A (PKA), which phosphorylates various proteins to modify their activity ( kinases phosphorylate things, dephosphorylases remove phosphates from things). The active βγ complex activates adenylyl cyclase, causing cyclic adenosine monophosphate (cAMP) production, which activates PKA. Both β 1 and β 2 receptors work through this pathway—each phosphorylating proteins that in turn cause their intended effects ( Fig. 7-7B ).
-
G i : Luckily this one is easy—it inhibits adenylyl cyclase, preventing cAMP production and PKA activation. G s stimulates cAMP production; G i inhibits.
